An Evaluation of our Program ‘Inspire Now’ – An Integrative Program of Yoga, Education, and Group Support

People with cancer and cancer survivors often have supportive care needs that aren’t fully met. Supportive care refers to services and treatments that help people manage the physical, emotional, and practical effects of cancer. One study highlighted that 75% of patients reported at least one unmet supportive care need, with the most common being information needs (58%) (e.g., information about cancer and available treatments), and psychological needs (51%) (e.g., emotional distress, help coping, and improving anxiety and depression) (1). In lung cancer, unmet supportive care needs are linked with poorer quality of life (2). In order to support people living with lung cancer, the Patterson Institute for Integrative Oncology Research (in partnership with the Centre for Health Innovation) runs a program called Inspire Now – A Program for People with Lung Cancer.
This blog provides an overview of the paper: Enhancing Quality of Life in People with Lung Cancer: An Integrative Program of Yoga, Education, and Group Support, which is an evaluation of the “Inspire Now” program. To enhance readability and understanding, words in bold are defined at the end of the post.
What is the Inspire Now program?
The Inspire Now program is open to anyone with a past or present diagnosis of lung cancer, as well as for people with other cancers that have spread to the lungs (lung metastasis). It was developed primarily by Anne Pitman, a certified yoga therapist, with input from naturopathic doctors at the CHI and two patient advocates. The program is offered virtually and free of charge.
The program is six weeks long, with one 2.5-hour class each week. Classes are facilitated by Anne and consist of four parts:
- Group check-in, support, and discussion,
- An educational talk from practitioners at the CHI exploring various topics related to mental and physical wellness for people with lung cancer and lung metastasis,
- Gentle yoga and breath practice, and
- A final group check-in.
How was the study designed?
This was an observational study in people with lung cancer who attended the Inspire Now program. Anyone who registered for the program was eligible to take part in the study. Our primary goal was to determine whether the program affected quality of life. We also evaluated overall wellbeing, personal concerns, program satisfaction, and overall experience. This was done by administering a set of questionnaires before the program started (called a baseline assessment) and after it ended (called a follow-up assessment).
We looked at how each person’s questionnaire scores changed from the start of the program (baseline) to the end of the program (follow-up). If a person’s score improved, it means they felt better in that area. We also gathered open-ended information from participants (called qualitative research). We reviewed this information for common ideas or patterns. If enough people mentioned the same idea, we call it a “theme.” These themes help us understand the shared experiences and concerns of participants.

What were the results?
We collected data from 31 program participants. Most participants identified as female (87%), had stage IV lung cancer (68%), and were currently receiving conventional cancer treatments (74%).
Quality of life, overall wellbeing, and personal concerns were all improved
We saw both statistically significant and clinically significant improvements in quality of life, wellbeing, and personal concerns from baseline to follow-up. In other words, compared to before the program, we are confident that quality of life, wellbeing, and personal concerns were all improved in meaningful ways for these participants after the program ended. Table 2 from the paper is included below for those who are curious to see the data and enjoy reading and analyzing research.
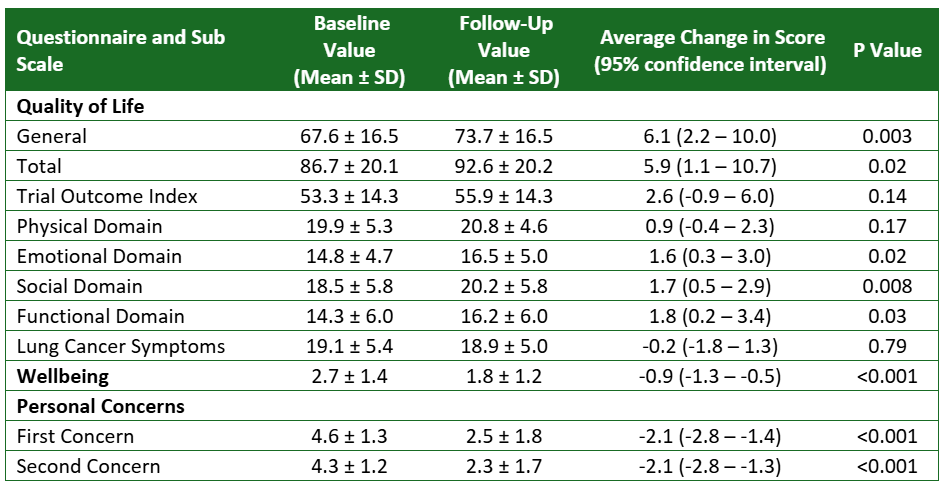
For those of you interested in learning what these numbers mean, here is a relatively simplified explanation. If you aren’t interested in this, skip to the next section!
Let’s look at the first line of the table. The first column shows the name of the questionnaire (quality of life – general) and the next two columns show the average scores (mean and standard deviation) of all 31 participants before and after the program. The following column shows the average change in score after the program. In this example, the average score went from 67.6 before the program to 73.7 afterwards—an increase of 6.1 points. But this number is just an estimate, so we calculate a 95% confidence interval to show how sure we are. This means we are 95% confident that the true change is somewhere between 2.2 and 10 points. The next number, called the P value, is 0.003—which is less than 0.05—so we call this result statistically significant. This gives us more confidence that the improvement we see in scores is real.
Participants most valued the connections they made and the knowledge they gained
The two most important aspects of the program participants reported were 1) connecting with others (mentioned by 61% of participants) and 2) obtaining knowledge and information (mentioned by 32% of participants). Participants spoke to feeling supported during the classes, both from other participants and from the program facilitator. Many specifically mentioned connecting with others who shared their own experiences with lung cancer as being important. One participant said:
“I loved being able to share our true feelings and frustrations in a safe and supportive environment. I must say the 2 hours and 30 minutes flew by and I really looked forward to this time spent with others going through the same disease of lung cancer. It is so helpful to have people who aren’t just sympathetic but empathetic.”

Participants also valued what they learned during the program, whether it was from the planned education sessions, thoughts and techniques offered by the facilitator, or learning from other participants. Here is one quote that relates to this:
“The educational piece was really important to me. If I wanted to know more about any subject, I could deep dive it on my own after.”
Importantly, we used an open-ended question to gather this data: what was the most important aspect of the program for you? Using non-leading questions is important as leading questions can influence the way participants describe their experiences.
The virtual format received positive feedback
We also asked participants how they felt about the program being conducted virtually. Everyone responded positively. The most common theme was that it made the program more convenient and accessible, which was mentioned by 45% of participants. Another minor theme identified was an increase in comfort (13%), meaning participants felt more comfortable sharing their experiences in their own home. Although this is encouraging, it is important to remember that people knew the program would be virtual before they signed up. This means that if someone knew they would not enjoy a virtual program, they would likely not sign up.
What are the conclusions?
The Inspire Now program can be an option to help address some of the most important unmet supportive care needs of people with lung cancer and lung cancer survivors. Because the program is free and home-based, it is accessible to people from across Canada. Studying programs like this in a research setting is important because it measures the effects in a clear, scientific way. This information can guide future improvements and show the wider scientific community that these programs are valuable. One important limitation of our study is that we did not follow participants over the long term, so we cannot say whether the positive changes would last.
Future Research
Because of the success of this study, we have started an evaluation of another one of our programs: Head Start. This program is available (virtually and free of charge) to people newly diagnosed with breast cancer. Although there are slight differences in the questionnaires we are using, the basic idea of the study is the same. We are also learning from our evaluation of the Inspire Now program, as we are conducting a longer-term follow-up to see if any changes we see are sustained over time.
How to take part in the Inspire Now program
The Inspire Now program is offered through the Centre for Health Innovation, via an online platform. The program is usually offered 3 times per year, is free of charge, and is open to anyone in Canada with a lung cancer diagnosis or to people who might have another cancer that has spread to their lungs. If you, or someone you know meet these criteria, you can find out more information on the program here.
Definitions
Observational study: when researchers watch and collect information about people or situations without changing anything or giving them something to take (for example, experimental treatments). This type of study design involves simply observing and documenting what happens to find patterns or relationships.
Clinical significance: a change or result that is big enough to have a noticeable impact on a person's health or daily life. For example, if pain goes down by 2%, that probably isn’t meaningful to a person, but if pain goes down by 40%, that likely is, Researchers have specific methods to determine what is likely a meaningful change.
Statistical significance: a tool researchers use to see if their results are likely to be reliable or just due to random chance. It doesn’t prove something is definitely true; instead, it gives a number (the P value) that helps determine if the findings are strong enough to suggest a real effect. Usually, P values less than 0.05 are classified as statistically significant.
Confidence interval: a range of numbers that shows how sure researchers are about their result. For example, if a 95% confidence interval is 5 to 10, researchers are 95% sure that the real number is somewhere between 5 and 10.
Follow the Patterson Institute for Integrative Oncology Research on socials for more:

Mark is a full-time research coordinator with the Patterson Institute for Integrative Oncology Research. He is involved in the development, implementation, day-to-day activities, and publication of all research conducted at the CHI. Mark joined Dr. Dugald Seely, ND’s research team in 2018 after volunteering with his brother, Dr. Andrew Seely, at The Ottawa Hospital. Mark is also an employee of The Ottawa Hospital Research Institute, a Certified Clinical Research Professional (CCRP), and an active member of both the Canadian College of Naturopathic Medicine and Ottawa Health Sciences Network Research Ethics Boards.
References
- Springer F, Mehnert-Theuerkauf A, Gebhardt C, Stolzenburg JU, Briest S. Unmet supportive care needs among cancer patients: exploring cancer entity-specific needs and associated factors. Journal of cancer research and clinical oncology. Apr 12 2024;150(4):190. doi:10.1007/s00432-024-05715-4
- Cochrane A, Woods S, Dunne S, Gallagher P. Unmet supportive care needs associated with quality of life for people with lung cancer: A systematic review of the evidence 2007-2020. Eur J Cancer Care (Engl). Jan 2022;31(1):e13525. doi:10.1111/ecc.13525
CHI Services
All Services
Supportive Cancer Care
Naturopathic Medicine
Acupuncture & TCM
Integrative & Functional Medicine
Nurse Practitioner Care
IV Therapy
Psychotherapy & Counseling
Grief Support
Hypnosis & Life Coaching
Yoga Therapy
Physiotherapy & Lymphatic Therapy
Osteopathy
Reflexology
CranioSacral Therapy
Massage Therapy
Nutritional Support & Meal Plans
Fees & Schedules
Please see our online booking site regarding fees and schedules.



